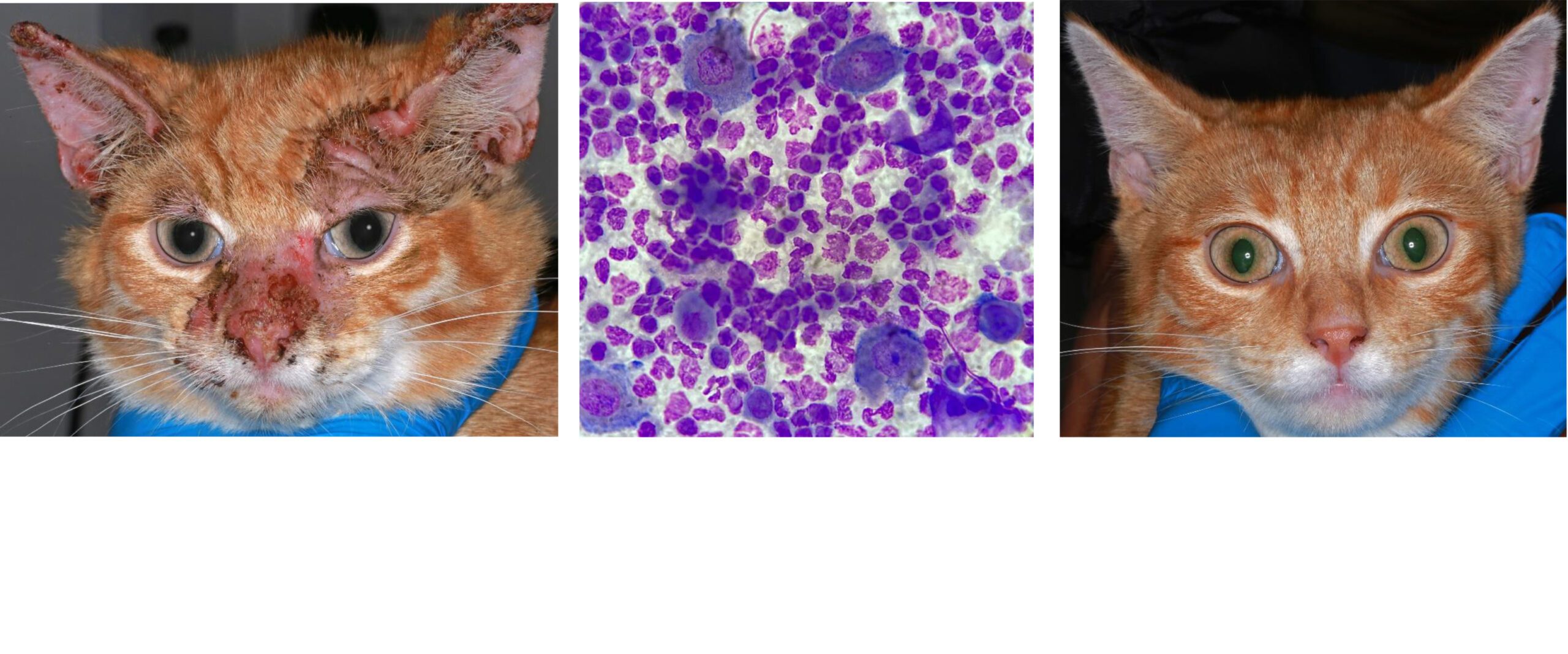
Pemphigus Foliaceus
The auto-immune condition I consult on most of all is Pemphigus Foliaceus (PF), in both dogs and cats. PF is most often idiopathic but can also be paraneoplastic (linked to internal malignancy) or iatrogenic (drug-induced). Other types of Pemphigus are much less common.
![]() Differential Diagnoses
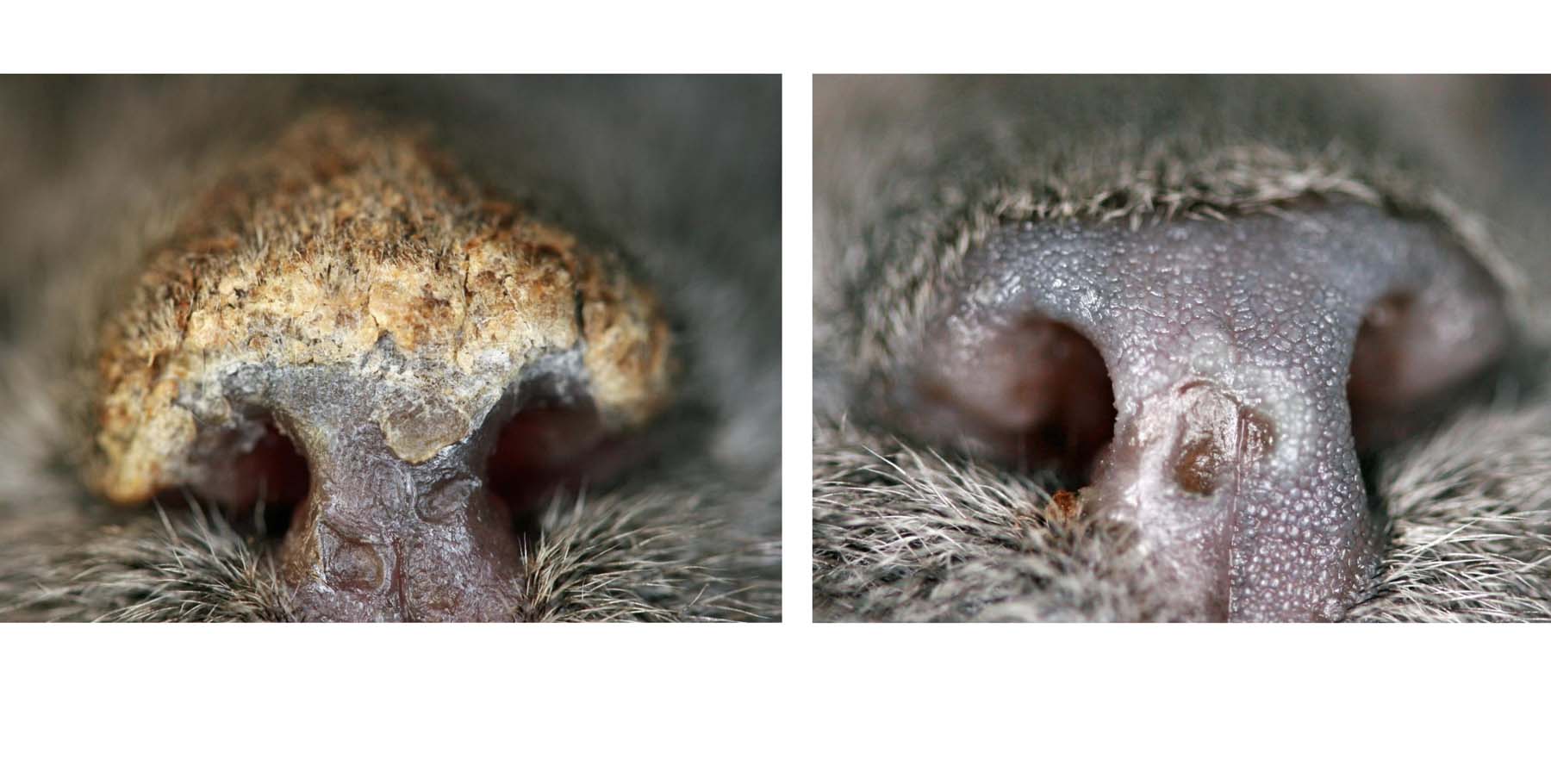
Differential Diagnoses
Auto-immune/Immune mediated: Pemphigus Erythematosus, Drug Eruption, Cutaneous and Systemic Lupus Erythematosus
Ectoparasitic: Demodectic mange (Demodex canis)
Fungal: Dermatophytosis (Trichophyton spp.)
Bacterial: Exfoliative Superficial Pyoderma (Staphylocccus pseudintermedius)
Protozoal: Leishmaniosis (Leishmania infantum)
Metabolic: Zinc-Responsive Dermatosis
Neoplastic: Epitheliotropic Lymphoma
![]() Pitfalls with Diagnosis
Pitfalls with Diagnosis
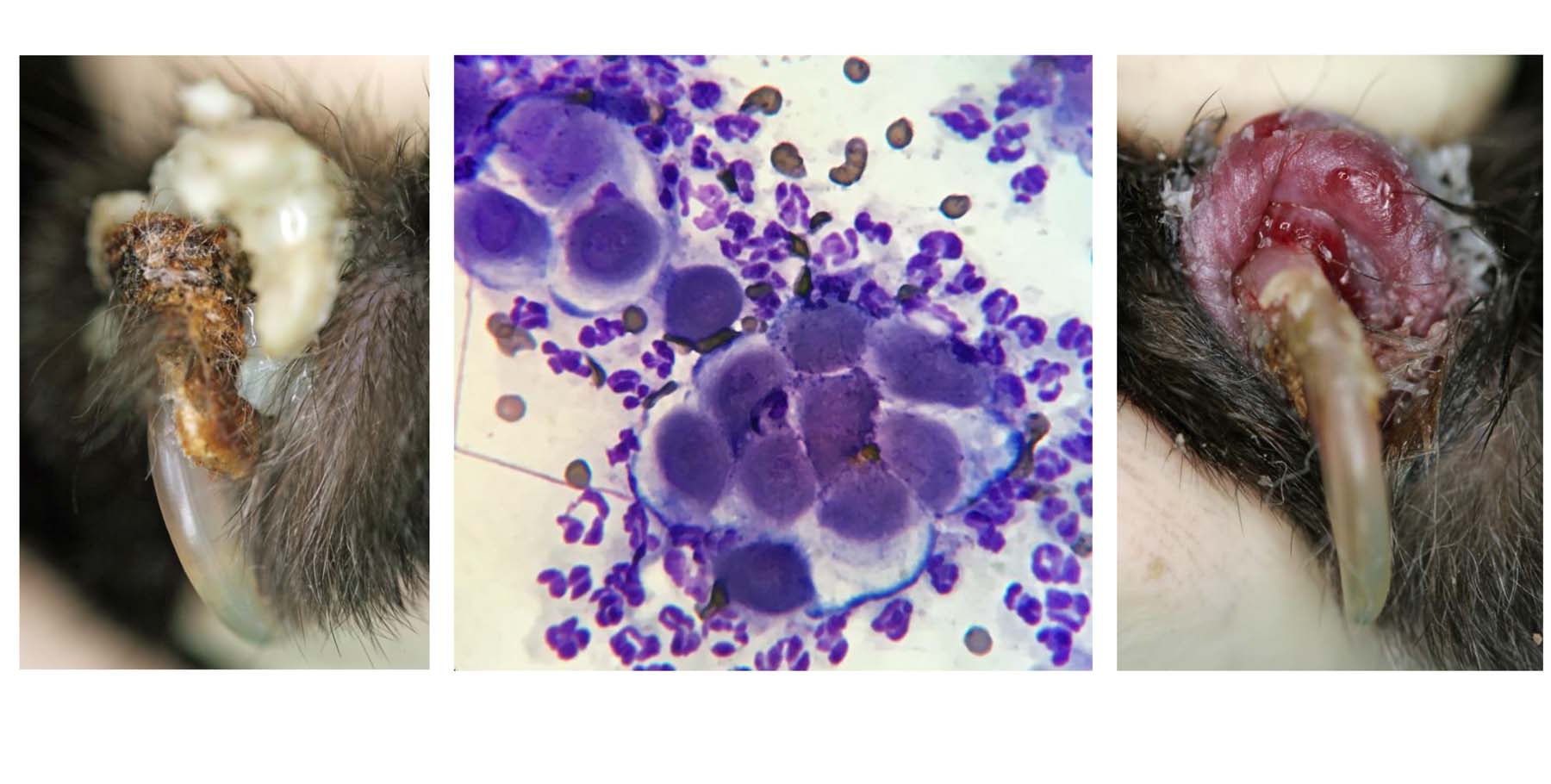
A combination of breed, age, clinical signs, lesion distribution and speed of progression, cytological appearance, co-morbidities and even reproductive status, should guide your diagnostic plan.
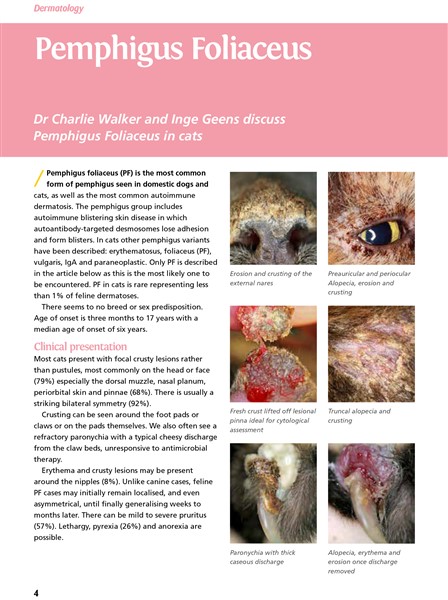
The presence of acantholytic keratinocytes and neutrophils, revealed on rapid in-house cytology, does not give a definitive diagnosis of PF – this combination of cells can be seen with bacterial and fungal infections too. PF may also present with concurrent secondary bacterial infection further clouding the cytological assessment.
External laboratory tests are often advisable to screen for triggering internal disease and unknown co-morbidities but also useful to check general baseline health prior to medication selection & ongoing use. Haematology, Biochemistry +/- Urinalysis would be the standard tests plus more recently Canine C Reactive Protein (and it seems likely Feline Amyloid A assays) may be recommended too. Screening for occult or concurrent infectious diseases may also be pertinent especially in travelled pets.
Differentiation from exfoliative superficial pyoderma or bullous impetigo, on first presentation, should involve consideration of the location of lesions, rapidity of expansion of the lesions, presence or absence of epidermal collarettes and scaling, plus the arrangement, size and shape of pustules. This should help to guide your diagnostic and management decisions. At least one biopsy sample must be stored deep frozen in the event that your pathologist suggests a tissue culture is necessary. This is not possible on formalinised samples and your client will not thank you for requesting a repeat biopsy procedure to collect more samples.
Differentiation from epidermolytic dermatophytosis (or pustular corneophilic dermatophytosis), especially Trichopyton spp., will be assisted by standard fungal culture, more rapid PCR as well as PAS staining of biopsies. This latter additional staining should be automatically offered by your pathologist when PF is a differential diagnosis.
Timing, lesion selection and handling of skin biopsies are very important. The opinion of a dedicated veterinary dermatohistopathologist on multiple, carefully selected, skin biopsies is paramount in making a confident diagnosis.
I am happy to receive referrals without any prior work up to allow prompt recognition, diagnosis and management. I also see cases whose diagnostic trail has faltered or those with almost definitive diagnosis when a treatment and management plan needs to be formulated.
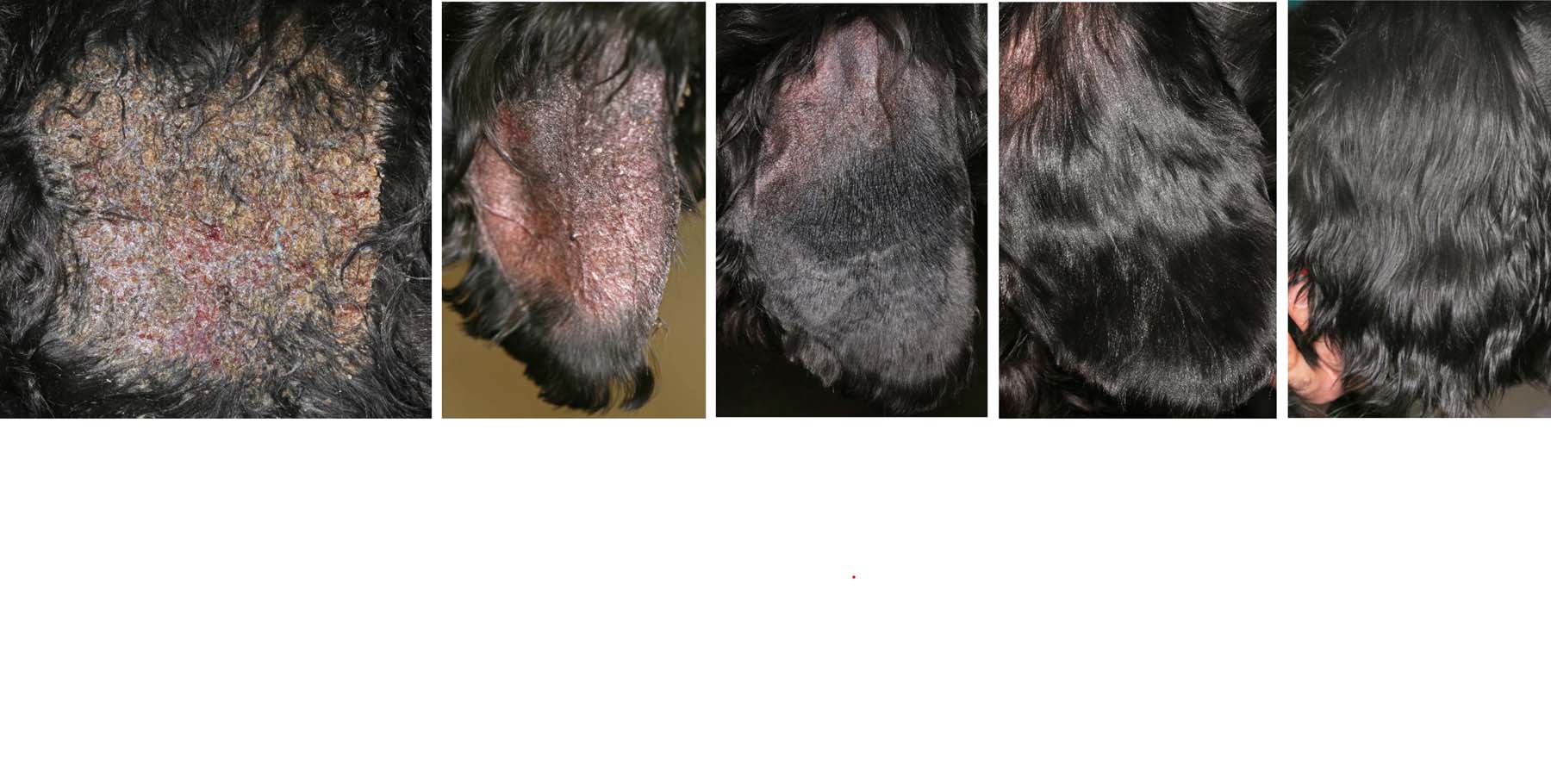
![]() Assessment of Severity and Response to Treatment
Assessment of Severity and Response to Treatment
A (canine) pemphigus foliaceus extent and severity index (PeFESI) has been proposed by Olivry and colleagues, at North Carolina State University, in order to quantify the degree of severity of the disease at initial presentation as well as the response to various treatment interventions. This scoring system consisted of the evaluation of the severity (0 none, 1 mild, 2 moderate and 3 severe) of the three cardinal lesions of PF (pustules, erosions and crusts) at 50 different areas covering the entire body surface.
![]() Treatment of Canine PF
Treatment of Canine PF
I offer a Very High Dose Glucocorticoid Induction, preferably in an in-patient basis, at least for the first pulse. The proportion of dogs achieving complete remission during the first twelve weeks of treatment is significantly higher than the standard high oral dose. This three day pulse also reduced the time to complete remission as well as the proportion of dogs needing adjuvant immunosuppression in the first twelve weeks. The great advantage with this new approach is that the oral steroid dose after the pulse is lower than with traditional inductions. Despite the very high dose used in this pulse method the number of dogs suffering significant side effects is no different to the those on traditional protocols. During each pulse, the dogs can be treated, assessed and monitored at Hospital practices that have round-the-clock nursing.
Many dogs will require adjuvant immunosuppressive medication.
Case series describing new, non-steroid, induction & maintenance therapies have been published since 2020. In some proven cases of PF, systemic steroid avoidance for patient reasons (concurrent Diabetes mellitus or Leishmaniosis for example) or pet parent concerns (corticophobia) may be possible.
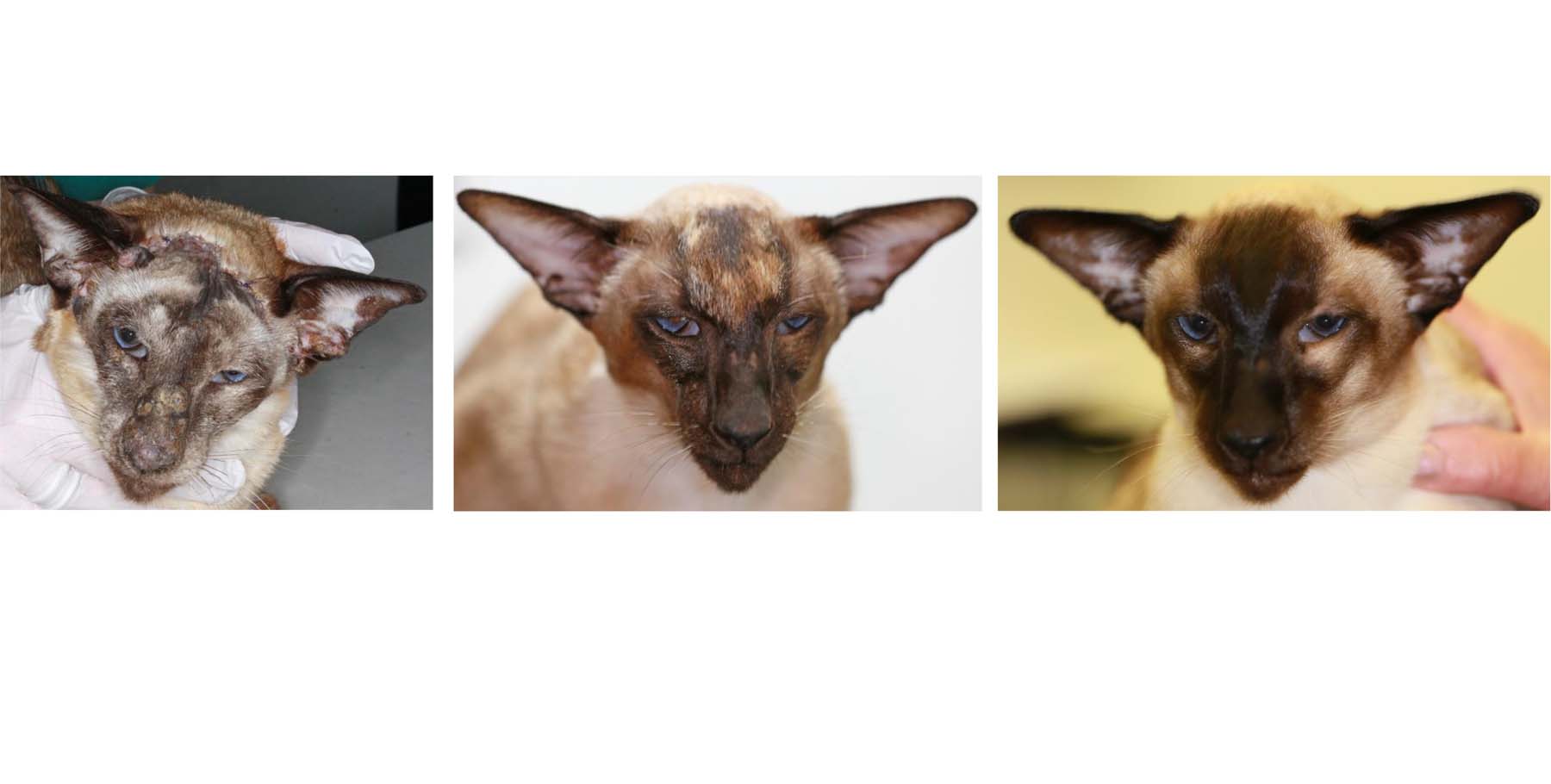
![]() Treatment of Feline PF
Treatment of Feline PF
To date, I have managed several cats, with localised PF, solely with specific topical glucocorticoid spray sometimes for several years. This causes no side effects and is not absorbed in to the cat’s body, unlike all other glucocorticoid preparations. This avoids oral, often troublesome, drug administration and is especially useful in cats that have cardiac disease or steroid-induced diabetes mellitus.
Invariably feline PF generalises and, most commonly I will then use liquid oral glucocorticoid to re-establish control (see Virbac’s 2017 Dermatology Case Book), Luckily there are now several palatable glucocorticoid tablets which remain as useful alternatives to a liquid in compliant cats.
Most cats do not require adjuvant immunosuppressive medication. Individual case reports describing new, non-steroid, induction & maintenance therapies have been published since 2021…
I co-authored an article on Feline PF, with Dr Inge Geens for CP/Clinic, Issue 2, 2016. This is a feline magazine for veterinary professionals published by Cats Protection.