Patient and Owner Compliance is paramount to controlling Otitis Externa
Ear disease (‘canker’, otitis externa) is a common, recurrent problem in many dogs, and some cats. Treating the secondary infections will often result in only a short to medium term resolution. Recurrence is very likely, if not inevitable, unless the primary cause is detected & treated.
In 2021, O’Neill et al, used anonymised veterinary clinical data from the VetCompass™ Programme to report the frequency of common disorders of dogs under primary veterinary care in the UK – a random sample of 22,333 (2.47 %) dogs from 784 clinics showed otitis externa was the second most common disorder. Click Here To Access
According to case files of more than 550,000 pets insured by a major pet insurance carrier, ear infection was the second most common claim filed in 2015*
Referral
In April 2019, at the North American Veterinary Dermatology Forum, Logas reported on treatment outcomes for canine chronic otitis externa in primary care vs referral dermatology practice settings. More dogs under dermatologist care experienced complete resolution of clinical signs (56% vs only 8%) & improved resolution of otic proliferative changes (95% vs 30%). The general conclusion was that these cases had better long term outcomes when treated by dermatologists, alongside primary care (‘GP’) vets, than those treated by GP Vets alone. Referral was recommended for otitis cases not resolving with treatment after 2 to 3 months.
With timely referral, before permanent painful ear canal changes have developed, I hope to:
![]() Control any established secondary infection, often without requiring ear wash-outs under general anaesthetic
Control any established secondary infection, often without requiring ear wash-outs under general anaesthetic
![]() Prevent further infections, with a simple, inexpensive, safe, proven lifelong regimen
Prevent further infections, with a simple, inexpensive, safe, proven lifelong regimen
A 2023 case example: ‘Buddy’, a five & a half year old Labrador Retriever, who has suffered 12 episodes of otitis externa with secondary infection, due to canine atopic dermatitis. The referring clinic’s staff & owners totalled his treatments to approximately £4,000.00 since the onset of his chronic recurrent ear inflammation, with the costs escalating rapidly with his worsening condition, so that £1000.00 was spent in the last 4 months before his first Dermatology Referral Consultation. He is now receiving a full-explained, multimodal, ongoing long term, treatment regimen but the two key, simple, safe, fortnightly treatments are likely to cost only ~£75.00 per annum. With continued compliance, these topical treatments will often fully control the inflammation & prevent any further secondary infections ever occurring again.
Conscious Video-Otoscopy
Whenever possible your pet’s ear(s) will be examined with a hand-held Firefly DE551 WiFi video-otoscope. This innovative device streams high quality live video (at 30fps) to my laptop or clinic TV, enabling us to view crystal clear images or videos of the ear canals. It is invaluable for allowing me, as well as the owner, to observe the extent of an otitis issue and very useful to monitor progress over time.
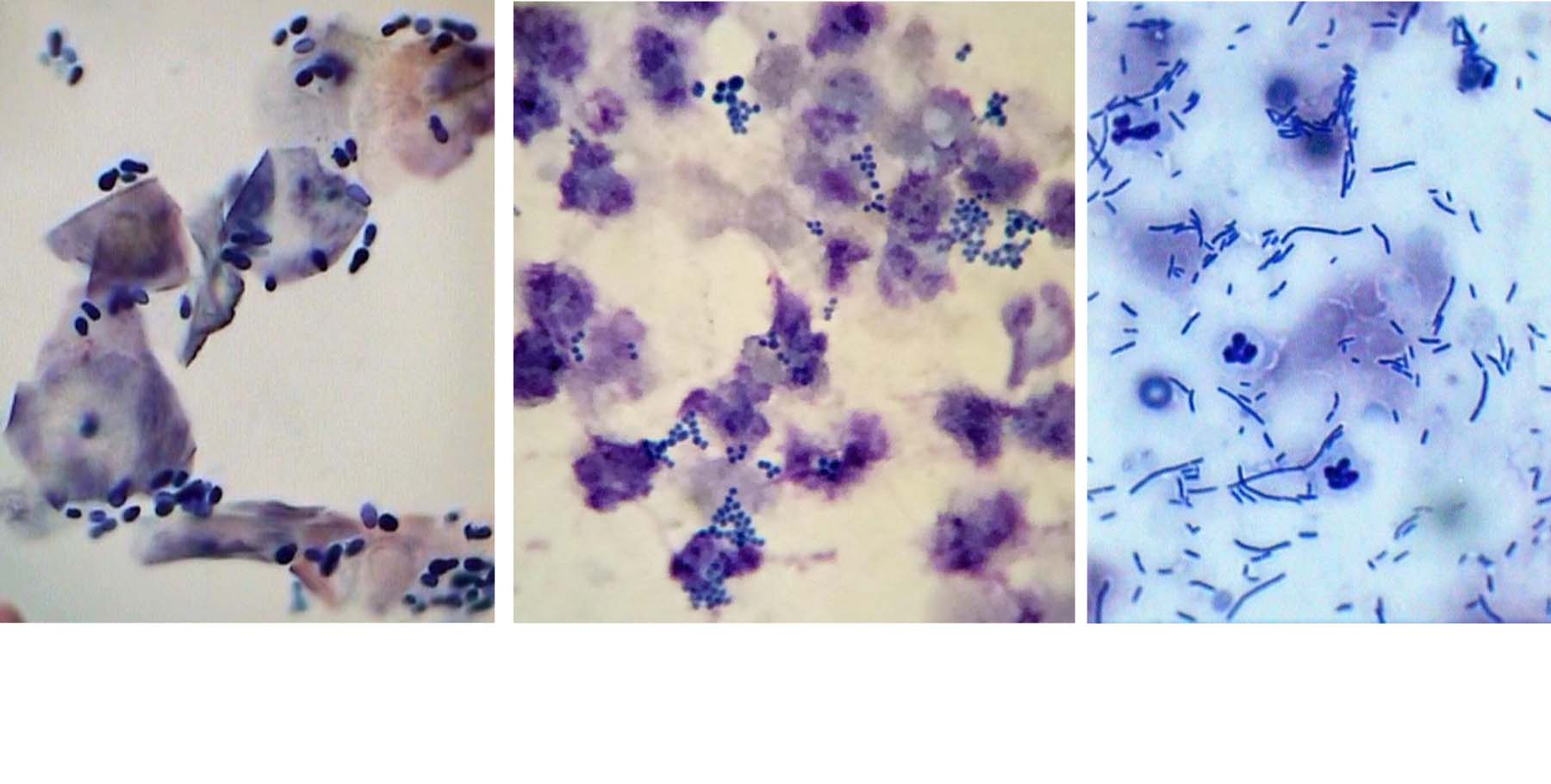
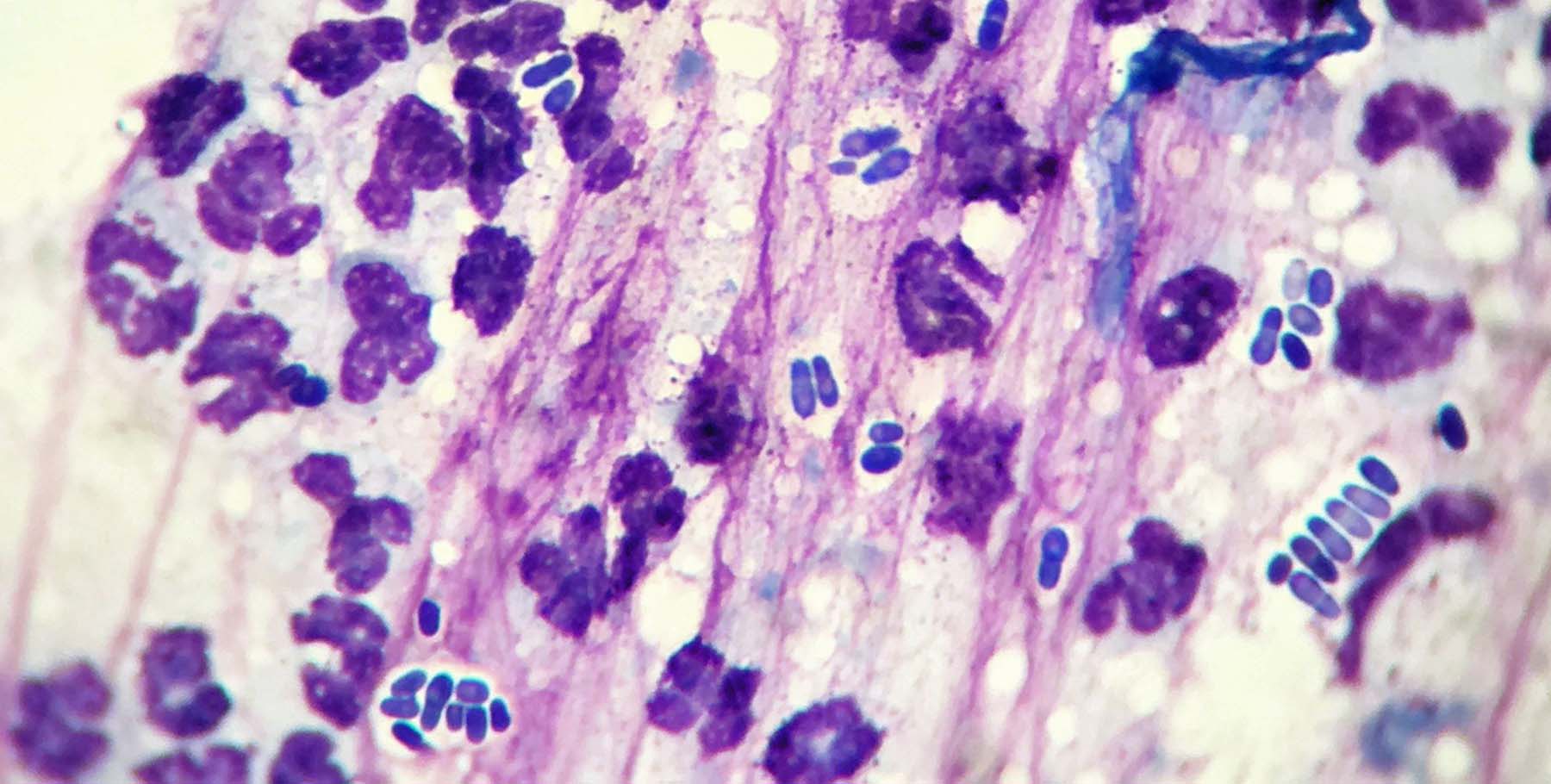
Cytology
The ear(s) may be inflamed only, or inflamed and infected with any combination of yeast, round or rod-shaped bacteria, and/or with parasites. By rapidly examining a stained ear wax preparation, I can immediately diagnose and ‘stage’ the degree of infection and inflammation. This allows us to decide on more specific diagnostic tests and targeted treatments. It also provides me with a rapid, accurate method of monitoring the response to previous, recent treatments.
As with itch scoring, a scoring system for Otitis is now being developed – here is a 2014 publication free to access through Wiley On-line: A Pilot Study to develop an Objective Clinical Score for Canine Otitis Externa. Veterinary Dermatology. Volume 25: Issue 6: Pages: 530-e92 Tim Nuttall & Emmanuel Bensignor
Microbial Cultures…?
Most cases that are referred to me have had expensive, often repetitive, microbial cultures and sensitivity tests on their aural discharge. Studies have documented various challenges associated with otic cultures – firstly a lack of reproducibility. Numerous studies have shown that samples collected from the same location in the ear, at the same time, show different results — either different organisms or the same organism with a different susceptibility pattern. Secondly lack of predictability – in canine otitis externa, caused by so-called resistant bacteria, the correlation between culture results and response to treatment is poor. The discordant results between bacterial culture, and subsequent sensitivity testing, and clinical response can be explained by the fact that the concentration of antimicrobial in the topical otic medication is up to 1000× the concentration of the antimicrobial that is tested in vitro. The sensitivity testing predicts that the organism will be resistant to the much weaker concentration of medication in the bloodstream. This means that the organisms classed as ‘resistant’ should be killed by the tested antimicrobials because they are in much much higher concentrations in the ear than in the bloodstream. The secondary infection is more likely not to have responded for several other reasons such as poor pre-treatment cleansing of the ear canal, patient incompliance, the organism’s protective biofilm, inadequate concurrent anti-inflammatory medication and so on.
If either a rod-shaped bacteria, with or without neutrophils (white blood cells), have been seen on point-of-care cytology &/or profuse Pseudomonas (silent ‘P’) or Proteus bacteria has been cultured from your dog’s ear(s), then your GP Vet should be advising you on a lifelong, non-antibacterial medical regimen, ideally including the offer of referral to a dermatologist. Once this infection has been encountered, it is essentially guaranteed to recur unless the primary cause has been diagnosed & an individualised, multimodal, management protocol has been devised. Repeated infections will eventually establish recalcitrant, resistant bacterial infection which will eventually require radical salvage surgery to resolve.
Oral Antibacterials…?
There is no current evidence supporting the use of oral (systemic) antibiotic therapy in the treatment of otitis externa in dogs. There is also no evidence that systemic antibiotics alone or in combination with topical preparations can improve treatment outcome, as compared with use of topical antibiotics alone. A significant problem associated with their administration is to promote the evolution of multi-resistant bacteria.
Pain Relief!
Because inflammation is a common component of canine otitis externa, topical steroids can be beneficial. If inflammation of the ear canal is severe, or if the canal is stenotic, additional therapy with oral steroids can help expedite clinical response, even in the case of serious secondary infection.
Otitis externa is often painful, and unfortunately dogs may hide pain, especially if otitis is chronic or recurrent. It is important not to overlook the need for use of systemic analgesics (oral painkillers) during episodes of otitis. I may advise that your dog is given a safe combination of 2 human medications twice prior to our consultation to ensure that I am able to examine the ears fully without causing pain & distress. It is very common to see dogs becoming head shy & even uncharacteristically aggressive during attempts at ear examination & treatment due to the often unmanaged pain & discomfort which always accompanies aural inflammation.
For the further information on canine otitis externa I would recommend Dechra’s www.ear-inflammation.co.uk/ & their interactive www.4d-earmodel.com/ .
For further information about an exciting new treatment modality see Fluorescence-biomodulation-trial
The PPPS System
The factors, causing ear canal inflammation & infection, can be divided into three categories – primary, predisposing, perpetuating & secondary – listed below. Examples of the most common causes are given:
Primary causes
These factors directly induce ear inflammation (otitis externa):
Hypersensitivity ![]()
Atopic dermatitis (the most common cause), Adverse Food Reactions (food allergy or dietary intolerance), Contact hypersensitivity
![]() Parasites
Parasites
Mites – Ear Mites Otodectes cynotis, ‘Fox’ mange Sarcoptes scabiei, Demodex canis mites
Ticks & fleas Echidnophaga gallinacea, Spilopsylla cuniculi
![]() Foreign bodies – Grass seeds/awns, loose hair, sand, dirt, medication concretions (grooming powders)
Foreign bodies – Grass seeds/awns, loose hair, sand, dirt, medication concretions (grooming powders)
![]() Keratoseborrhoeic – Hypothyroidism, Primary idiopathic seborrhoea, Vitamin A – responsive Dermatosis
Keratoseborrhoeic – Hypothyroidism, Primary idiopathic seborrhoea, Vitamin A – responsive Dermatosis
![]() Local Glandular disorders – Ceruminous gland hyperplasia, Sebaceous gland hyper- or hypoplasia, Altered secretion rate, Altered type of secretion
Local Glandular disorders – Ceruminous gland hyperplasia, Sebaceous gland hyper- or hypoplasia, Altered secretion rate, Altered type of secretion
![]() Autoimmune diseases – Pemphigus foliaceus and erythematosus, Lupus erythematosus, Cold agglutinin disease, Epidermolysis bullosa acquisita, Vasculitides
Autoimmune diseases – Pemphigus foliaceus and erythematosus, Lupus erythematosus, Cold agglutinin disease, Epidermolysis bullosa acquisita, Vasculitides
![]() Microorganisms – ‘Ringworm’ (Dermatophytosis) Microsporum canis etc
Microorganisms – ‘Ringworm’ (Dermatophytosis) Microsporum canis etc
![]() Viral – Distemper
Viral – Distemper
![]() Inflammatory – Frostbite & solar (actinic) dermatitis – white cats & dogs, Juvenile cellulitis, Eosinophilic dermatitis-granuloma, Sterile eosinophilic folliculitis, Relapsing polychondritis, Nasopharyngeal polyps
Inflammatory – Frostbite & solar (actinic) dermatitis – white cats & dogs, Juvenile cellulitis, Eosinophilic dermatitis-granuloma, Sterile eosinophilic folliculitis, Relapsing polychondritis, Nasopharyngeal polyps
Predisposing factors
These increase the risk of development of ear disease but do not directly induce it:
![]() Conformation – Long, dangling ear flaps (pendulous pinnae), Hairy ear canals (hirsutism), Stenotic canals
Conformation – Long, dangling ear flaps (pendulous pinnae), Hairy ear canals (hirsutism), Stenotic canals
![]() Excessive moisture – ‘Swimmer’s ear’, High humidity environment
Excessive moisture – ‘Swimmer’s ear’, High humidity environment
![]() Excessive cerumen (wax)
Excessive cerumen (wax)
![]() Obstructive disease – Benign cutaneous neoplasia, Polyps
Obstructive disease – Benign cutaneous neoplasia, Polyps
![]() Treatment effects – Hair plucking (Groomers), Cotton bud trauma
Treatment effects – Hair plucking (Groomers), Cotton bud trauma
![]() Systemic disease – Immune suppression or viral disease, Generalised neoplastic or metabolic disease, Debilitation and negative catabolic states
Systemic disease – Immune suppression or viral disease, Generalised neoplastic or metabolic disease, Debilitation and negative catabolic states
Please note the first factor, conformation of the ear, does not directly cause ear disease. This is a common misconception. If this was true then all dogs with large, floppy, and/or hairy ears would have recurrent ear infections.
Perpetuating causes
These factors prevent resolution of the disease:
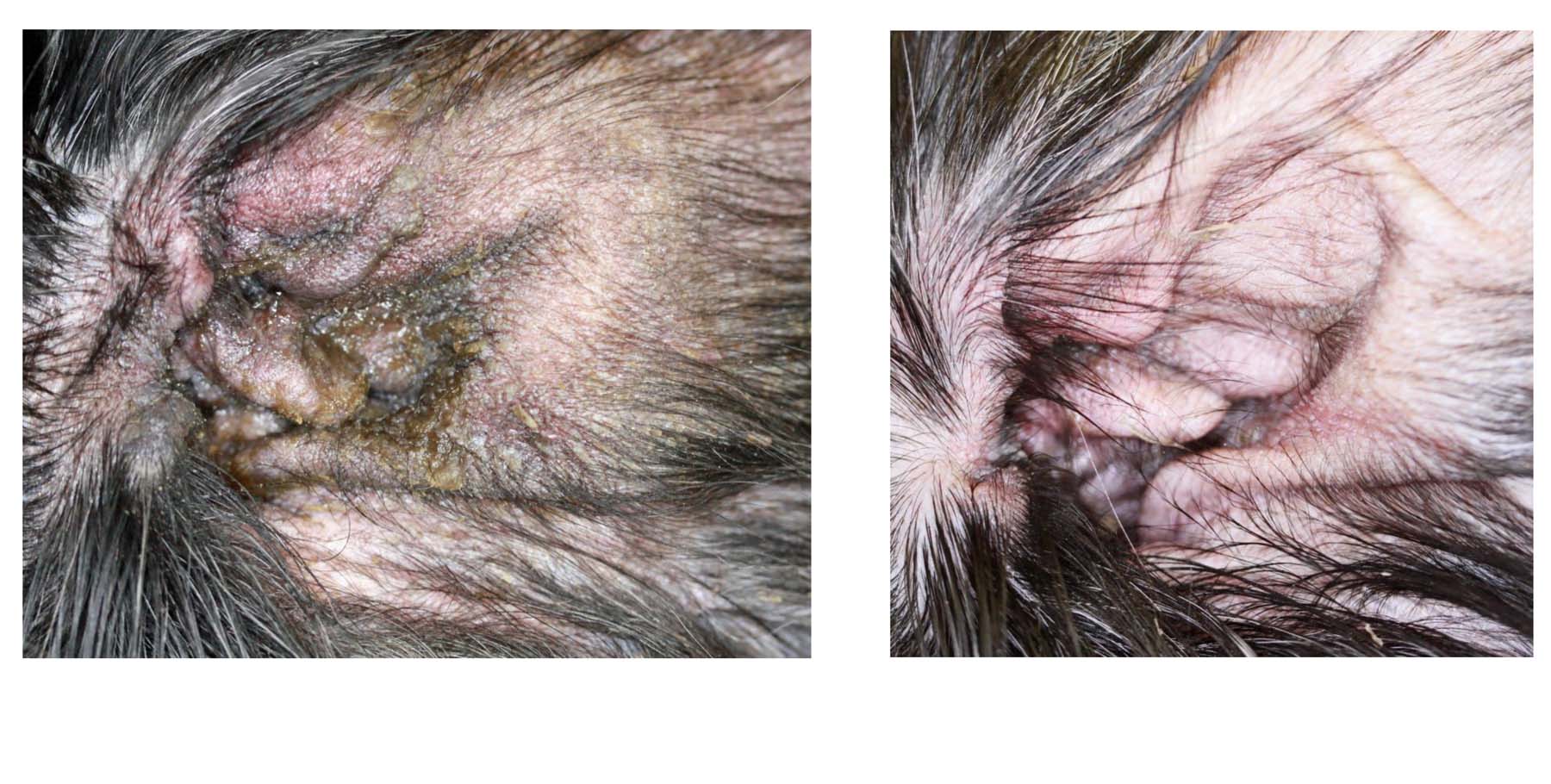
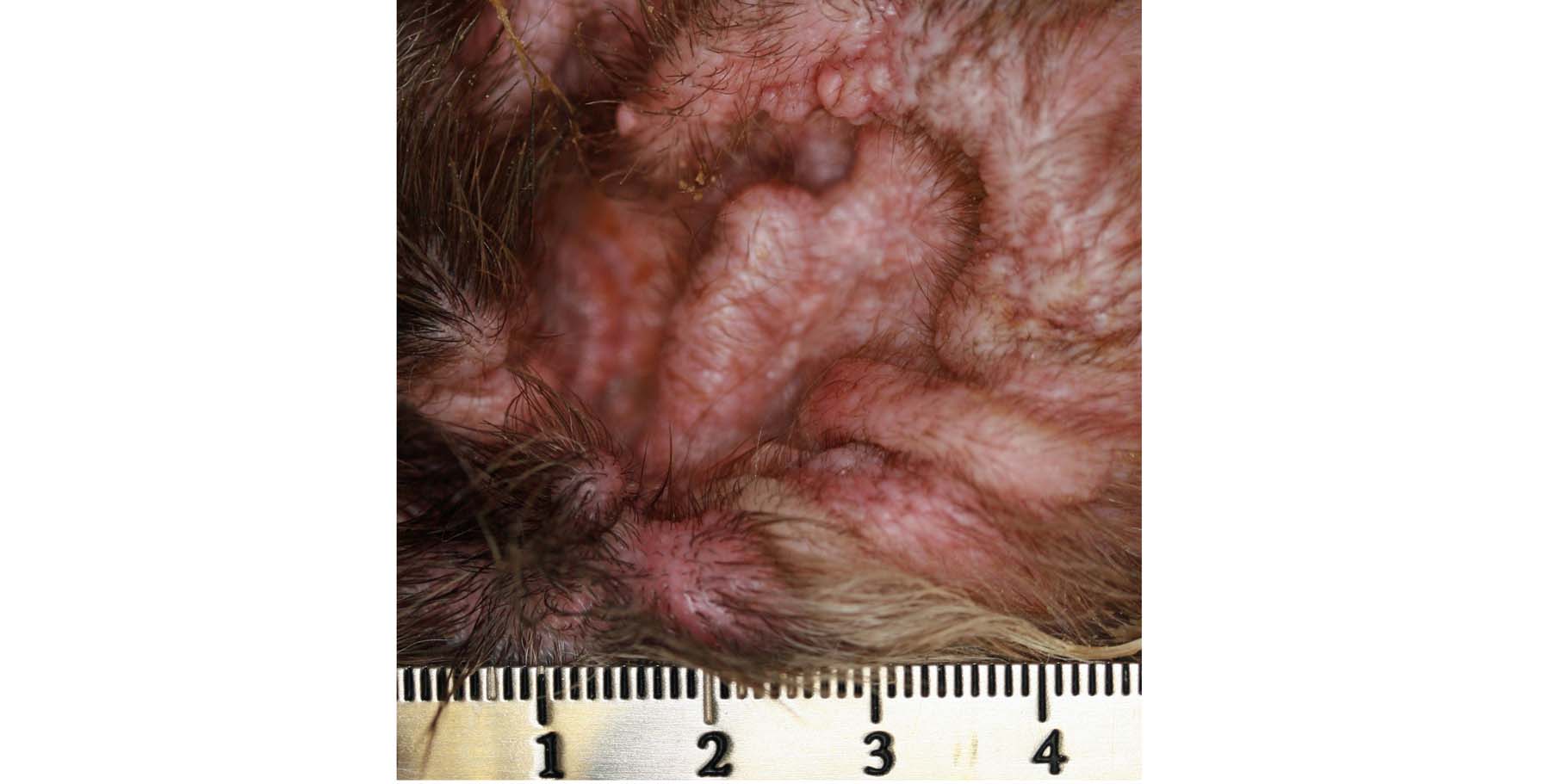
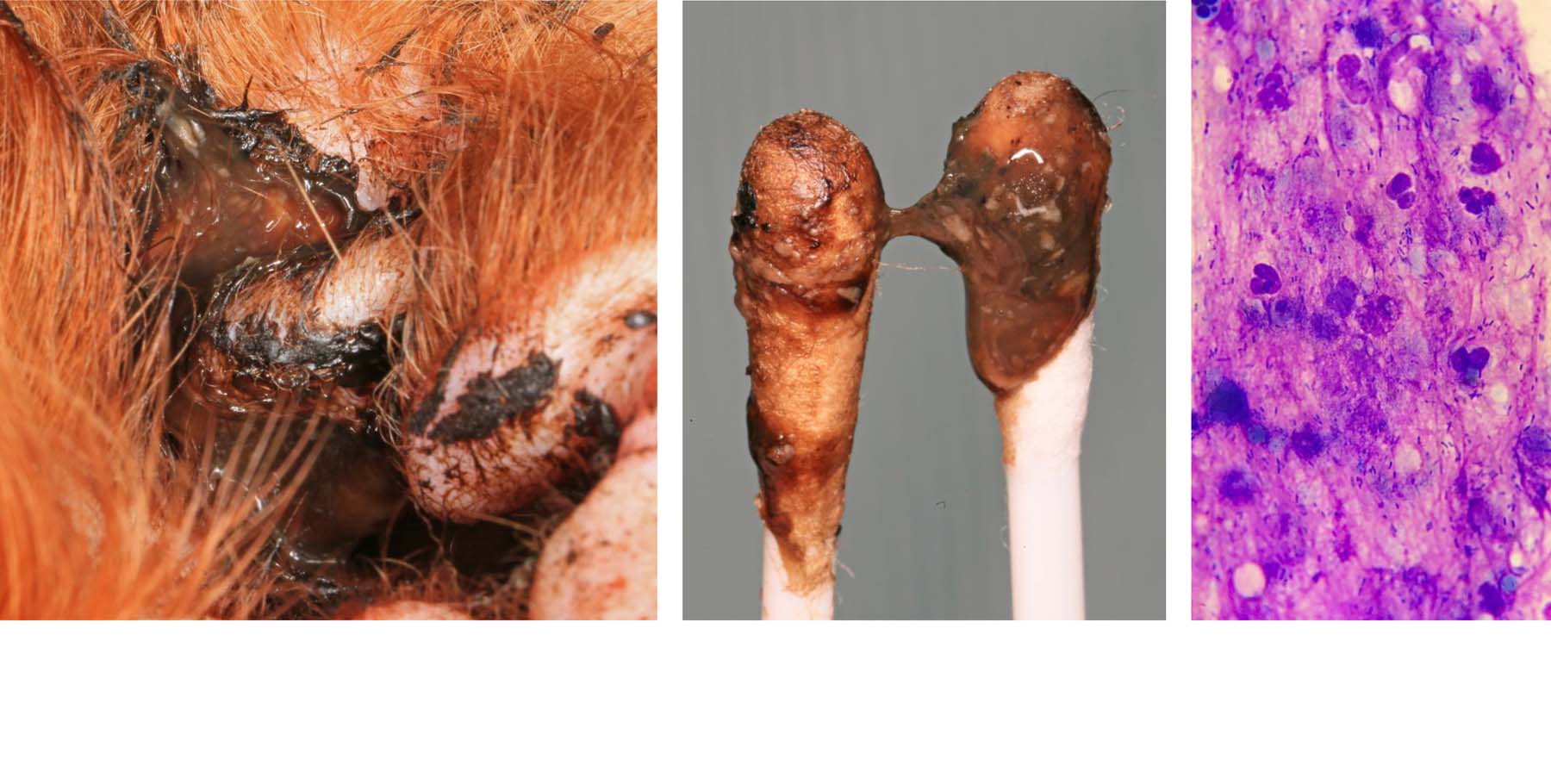
![]() Progressive pathological changes (from chronic inflammation and recurrent infections) – Ceruminous Gland hyperplasia, Disruption of elevator clearance mechanism, Fibrosis – scarring, Hidradenitis, Hyperkeratosis, Hyperplasia – increased epithelial folds, Oedema – swelling
Progressive pathological changes (from chronic inflammation and recurrent infections) – Ceruminous Gland hyperplasia, Disruption of elevator clearance mechanism, Fibrosis – scarring, Hidradenitis, Hyperkeratosis, Hyperplasia – increased epithelial folds, Oedema – swelling
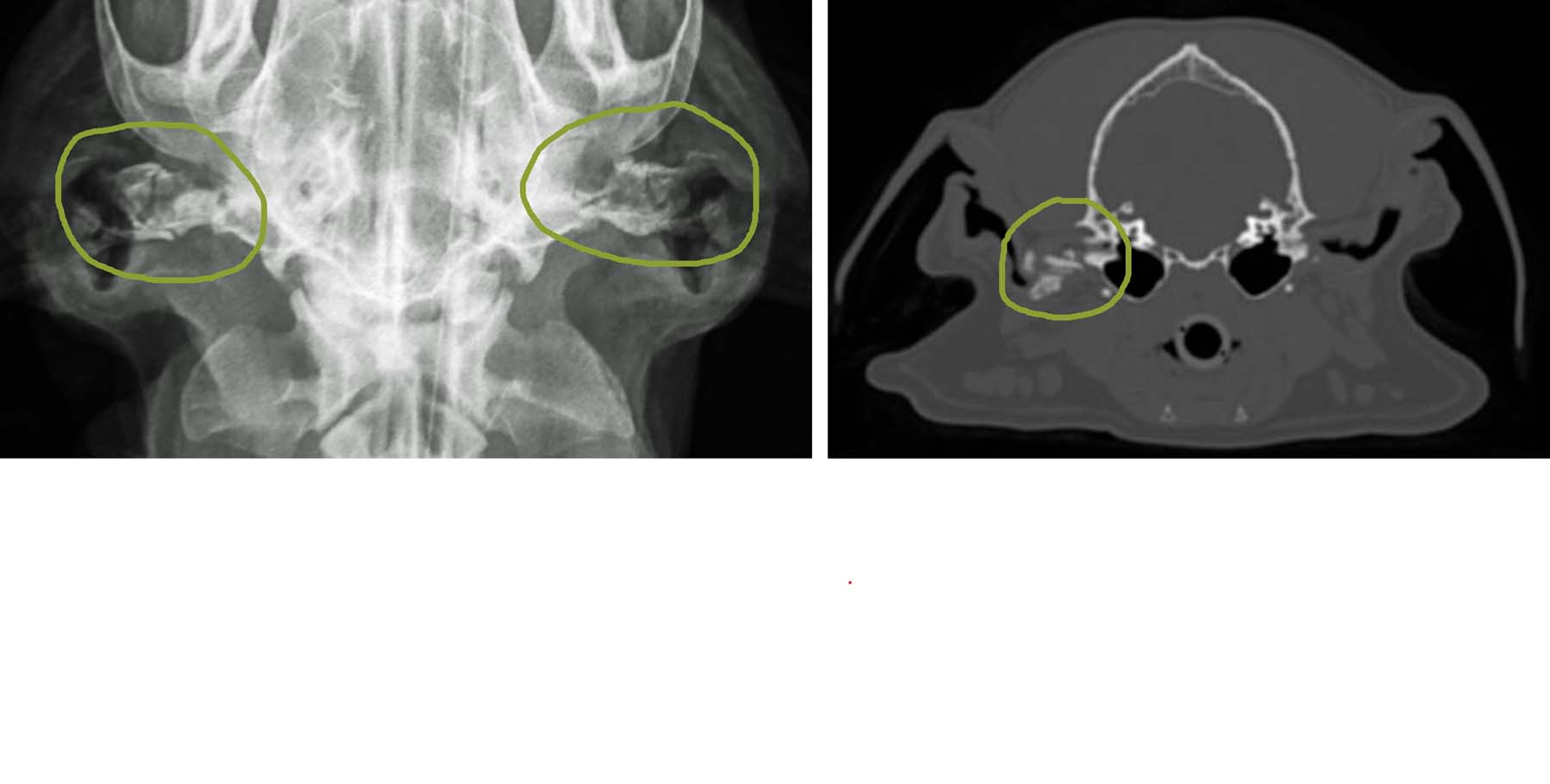
![]() Ossification of ear cartilage
Ossification of ear cartilage
![]() Otitis media (middle ear disease) – Simple purulent, Caseated or keratinous, Choleastoma, Proliferative or destructive osteomyelitis
Otitis media (middle ear disease) – Simple purulent, Caseated or keratinous, Choleastoma, Proliferative or destructive osteomyelitis
Secondary infections
Microbial infections, which are never primary, often cause the more acute clinical signs and this further progression leads to another visit to the Vet.
![]() Yeast – Malassezia pachydermatis, Candida sp.
Yeast – Malassezia pachydermatis, Candida sp.
![]() Bacteria – Staphylococcus pseudintermedius, (Streptococcus sp.), Pseudomonas sp. (Proteus sp., Escherichia coli etc.)
Bacteria – Staphylococcus pseudintermedius, (Streptococcus sp.), Pseudomonas sp. (Proteus sp., Escherichia coli etc.)
Therefore the more infections that a patient undergoes the more difficult it may be to reverse the progression of the ear disease.
Eventually permanent damage will ensue and surgical treatment will be the only option through re-referral to a Soft Tissue Surgeon for salvage surgery (total ear canal ablation with bulla osteotomy).
Download your Ear Infection Advice Sheet here: THE SKINVET RECURRENT EAR INFECTION INFORMATION SHEET
*Nationwide Pet (formerly Veterinary Pet Insurance). Identification of 10 most common medical conditions in dogs; based on database of more than 550,000 insured pets, as recorded 2015 veterinary visits. Brea, CA: Media release; March 24, 2016