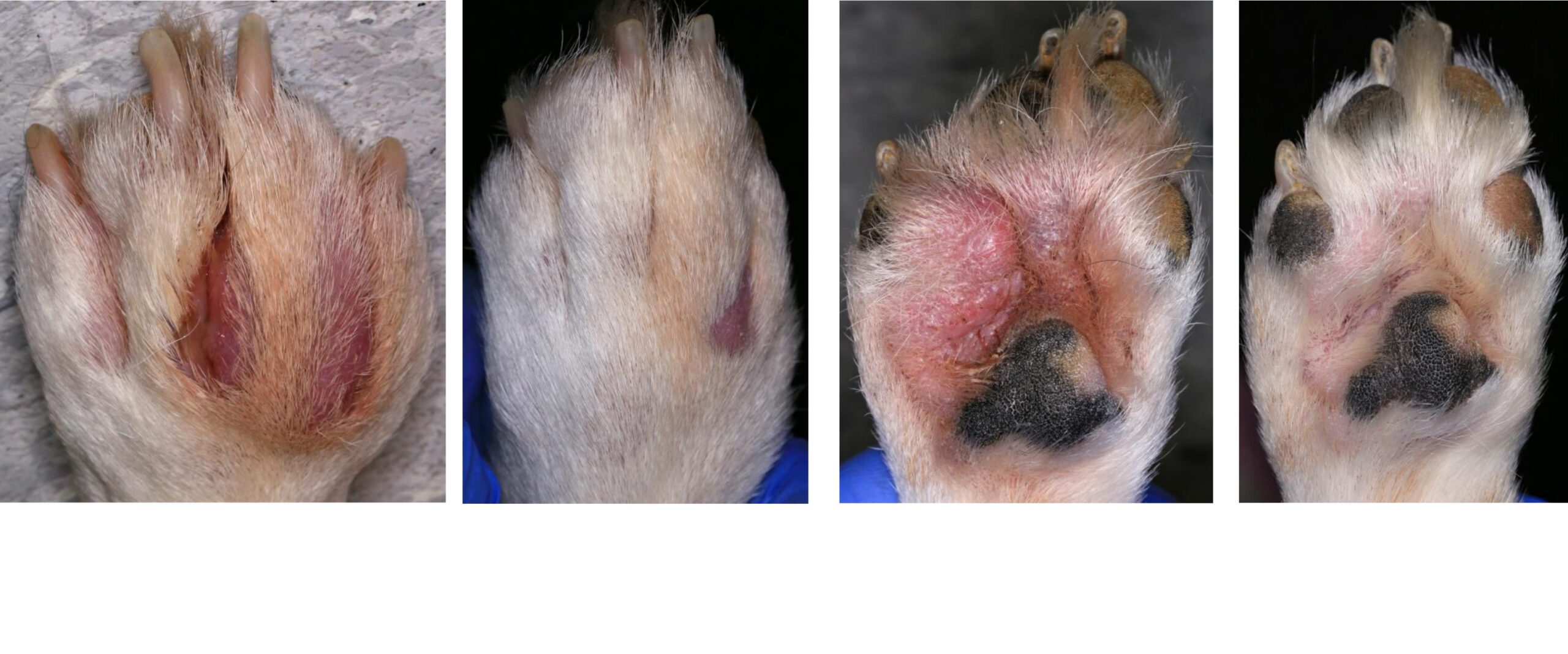
Interdigital ‘cysts’ are a common, recurrent and painful problem in many dogs. Treating the secondary infections will often result in only a short to medium term resolution. Recurrence is very likely unless the primary cause is detected & treated. The paw(s) may be inflamed only, or inflamed and infected with any combination of microbes (bacteria &/or yeasts), and/or with parasites.
The factors, causing Pododermatitis, digital and interdigital inflammation and infection, can be divided into four categories – primary, predisposing, perpetuating & secondary – listed below. Many of these factors, often in combination, can lead to the development of interdigital ‘cysts’.
I can work with you & your dog to formulate a long term, dedicated, multimodal medical treatment & management regimen which should provide good overall control of inflammation & infection, reduce flares including interdigital ‘cysts’ & very importantly provide pain relief, without repeated visits to your GP Vet & often unnecessary, long courses of oral antibacterials as recommended in the past.
For further information about an exciting new, adjunctive treatment modality see http://www.theskinvet.net/veterinary-surgeons/bacterial-pyoderma/fluorescence-biomodulation-trial
Primary causes
These factors directly induce paw inflammation (pododermatitis):
![]() Autoimmune Diseases – Pemphigus foliaceus (uncommon), Pemphigus vulgaris (very rare), Epidermolysis bullosa (very rare), Systemic lupus erythematosus (very rare)
Autoimmune Diseases – Pemphigus foliaceus (uncommon), Pemphigus vulgaris (very rare), Epidermolysis bullosa (very rare), Systemic lupus erythematosus (very rare)
![]() Cornification Disorders – Paw pad hyperkeratosis, Familial Hyperkeratosis
Cornification Disorders – Paw pad hyperkeratosis, Familial Hyperkeratosis
![]() Endocrine – Hypothyroidism, Hyperadrenocorticism
Endocrine – Hypothyroidism, Hyperadrenocorticism
![]() Foreign bodies Grass seeds/awns (very common), Thorns (hawthorn etc), Loose hair, stone, sand, salt etc
Foreign bodies Grass seeds/awns (very common), Thorns (hawthorn etc), Loose hair, stone, sand, salt etc
![]() Hypersensitivity Atopic dermatitis (common), Adverse food reactions (food allergy or dietary intolerance), Contact hypersensitivity (uncommon)
Hypersensitivity Atopic dermatitis (common), Adverse food reactions (food allergy or dietary intolerance), Contact hypersensitivity (uncommon)
![]() Immune-mediated Adverse Drug Reactions (uncommon), Dermatomyositis (rare), Idiopathic Sterile Granuloma/Pyogranuloma (uncommon), Lymphoplasmacytic pododermatitis (primary or chronic end-stage?) – Antibacterial-responsive (AbR-LPP) & Immunomodulatory-responsive (ImR-LPP), Plasma Cell Pododermatitis (cats), Symmetric Lupoid Onychodystrophy (or onychitis), Vasculitides (uncommon)
Immune-mediated Adverse Drug Reactions (uncommon), Dermatomyositis (rare), Idiopathic Sterile Granuloma/Pyogranuloma (uncommon), Lymphoplasmacytic pododermatitis (primary or chronic end-stage?) – Antibacterial-responsive (AbR-LPP) & Immunomodulatory-responsive (ImR-LPP), Plasma Cell Pododermatitis (cats), Symmetric Lupoid Onychodystrophy (or onychitis), Vasculitides (uncommon)
![]() Inflammatory – Reactive Histiocytosis
Inflammatory – Reactive Histiocytosis
![]() Metabolic – Calcinosis circumscripta, Hepatocutaneous Syndrome (Superficial Necrolytic Dermatitis), Vitamin A Responsive dermatosis, Xanthomas, Zinc Responsive Dermatosis
Metabolic – Calcinosis circumscripta, Hepatocutaneous Syndrome (Superficial Necrolytic Dermatitis), Vitamin A Responsive dermatosis, Xanthomas, Zinc Responsive Dermatosis
![]() Microorganisms – Bacteria esp. Mycobacteria (rare as primary cause), Dermatophytosis – Microsporum canis etc (uncommon), Malassezia Yeast (rare as primary cause)
Microorganisms – Bacteria esp. Mycobacteria (rare as primary cause), Dermatophytosis – Microsporum canis etc (uncommon), Malassezia Yeast (rare as primary cause)
![]() Multifactorial – Acral lick dermatitis
Multifactorial – Acral lick dermatitis
![]() Neoplasia – Fibrosarcoma, systemic/malignant Histiocytosis, Epitheliotropic Lymphoma, Mast Cell tumour, Melanoma, Soft Tissue sarcoma, Squamous Cell carcinoma, atrichial Sweat gland tumour, etc. & any metastases
Neoplasia – Fibrosarcoma, systemic/malignant Histiocytosis, Epitheliotropic Lymphoma, Mast Cell tumour, Melanoma, Soft Tissue sarcoma, Squamous Cell carcinoma, atrichial Sweat gland tumour, etc. & any metastases
![]() Orthopaedic – Congenital limb deformity, Cruciate disease, Degenerate joint disease/osteoarthritis, Elbow/Shoulder osteochondrosis dissecans
Orthopaedic – Congenital limb deformity, Cruciate disease, Degenerate joint disease/osteoarthritis, Elbow/Shoulder osteochondrosis dissecans
![]() Postural – Abnormal Gait/Conformation
Postural – Abnormal Gait/Conformation
![]() Parasites – Demodex canis mites (common), Hookworms (uncommon), Leishmaniosis (uncommon), Pelodera strongyloides (rare)
Parasites – Demodex canis mites (common), Hookworms (uncommon), Leishmaniosis (uncommon), Pelodera strongyloides (rare)
![]() Viral – Cowpox (cats), Distemper (rare), Papilloma
Viral – Cowpox (cats), Distemper (rare), Papilloma
Predisposing factors
These factors increase the risk of development of paw inflammation (pododermatitis) but do not directly induce it:
![]() Genetic – Short haircoat
Genetic – Short haircoat
![]() Obstructive disease – benign cutaneous neoplasia
Obstructive disease – benign cutaneous neoplasia
![]() Orthopaedic – Congenital limb deformity, Cruciate disease, Degenerate joint disease/osteoarthritis, Elbow/Shoulder osteochondrosis dissecans
Orthopaedic – Congenital limb deformity, Cruciate disease, Degenerate joint disease/osteoarthritis, Elbow/Shoulder osteochondrosis dissecans
![]() Physical – Excess bodyweight, Large & Giant breed dogs
Physical – Excess bodyweight, Large & Giant breed dogs
![]() Postural – Abnormal Gait/Conformation
Postural – Abnormal Gait/Conformation
![]() Systemic disease – Immune suppression, Generalised neoplastic disease, Debilitation and negative catabolic states
Systemic disease – Immune suppression, Generalised neoplastic disease, Debilitation and negative catabolic states
Some of these factors can be considered Primary too.
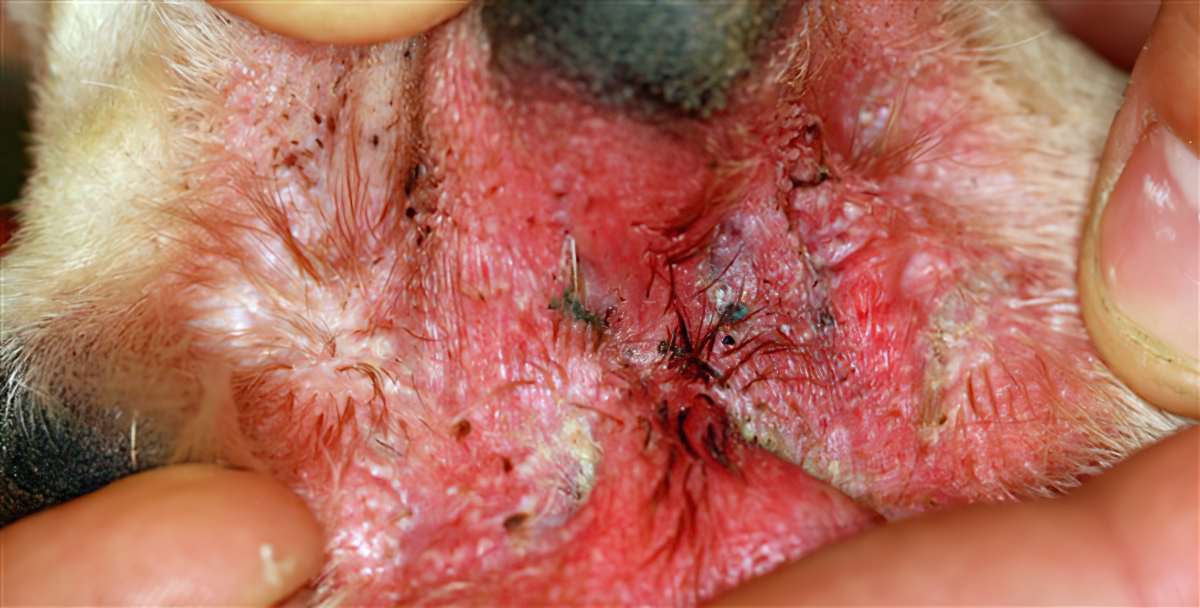
Increased weight bearing on haired palmar and plantar pad margins → tissue hypertrophy and hyperplasia → focal hairshaft trauma → furunculosis → subcutaneous keratin-driven inflammation (endogenous foreign body reaction)
Perpetuating causes
These factors prevent complete resolution of the disease, sometimes permanently.
![]() Chronic, severe lymphocytic-plasmacytic inflammation
Chronic, severe lymphocytic-plasmacytic inflammation
![]() Persistent endogenous foreign body reaction (keratin)
Persistent endogenous foreign body reaction (keratin)
![]() Progressive pathological changes (from chronic inflammation and recurrent infections) – Destructive osteomyelitis, Dermal fibrosis – scarring, Epidermal hyperkeratosis, Follicilitis and furunculosis, Glandular hyperplasia/dilatation, Hidradenitis, Hyperplasia and Hypertrophy – increased epithelial folds/abnormal new pad growth/conjoined pads; Oedema – swelling
Progressive pathological changes (from chronic inflammation and recurrent infections) – Destructive osteomyelitis, Dermal fibrosis – scarring, Epidermal hyperkeratosis, Follicilitis and furunculosis, Glandular hyperplasia/dilatation, Hidradenitis, Hyperplasia and Hypertrophy – increased epithelial folds/abnormal new pad growth/conjoined pads; Oedema – swelling
Secondary infections
Microbial infections, which are almost never primary, often cause the more acute clinical signs and this further progression leads to another visit to the Vet.
![]() Yeast Malassezia pachydermatis, Candida sp.
Yeast Malassezia pachydermatis, Candida sp.
![]() Bacteria Staphylococcus pseudintermedius, (Streptococcus sp.), Pseudomonas sp. (Proteus sp., Escherichia coli etc.)
Bacteria Staphylococcus pseudintermedius, (Streptococcus sp.), Pseudomonas sp. (Proteus sp., Escherichia coli etc.)
Therefore the more interdigital granulomas that a patient undergoes the more difficult it may be to reverse the progression of paw inflammation (pododermatitis).
Eventually permanent damage will ensue and surgical treatment will be the only option through re-referral to a Soft Tissue Surgeon for major salvage surgery (surgical laser ablation or fusion podoplasty).
Download your Interdigital Cyst Advice sheet here: TheSkinVet Recurrent Interdigital ‘Cysts’ Information Sheet (PPPS)